CoronaVirus
April 19th, 2020
Speaking as an immune compromised person, my message about CoronaVirus is:
- No vitamin, herb, supplement, homeopathic, aromatherapy, energy therapy, psychotherapy, drug, or vaccine can overcome the effects of an unhealthy lifestyle and poor quality sleep.
- We personally cannot afford to be unhealthy, to have unhealthy children-- or to live in unhealthy environments.
- Our Government cannot afford an unhealthy population— it is a security risk for one thing.
- We have work to do to insure a healthy future for ourselves, our children, our neighbors on planet Earth-- and our planet itself— so let's get busy!
My story in short: I have a rare genetic immune deficiency— Common Variable Immune Deficiency— (CVID). CVID is essentially a birth defect found in 1 of 30,000 people. Every 3 weeks Medicare and other insurance cover the $5,000.00 to $7,000.00 expense to boost my immune system with gamma globulins! I also have other related birth defects which are costly to insurance. I feel guilty about this expense, but cannot work to cover the costs myself~ so I hope to help prevent birth defects in others by educating about how a healthy lifestyle will make a HUGE difference.
It has been because of my very healthy lifestyle since my mid 30’s I have been able to live with these health conditions. I did not know I had CVID until 3 years ago— 32 years after major symptoms. So— I understand much about the immune system, and my message to readers here is that you want to avoid health problems as they are very time consuming and expensive— not to mention what they do to quality of life with resulting pain and limitation. I have been able to toughen up and become strong in other areas to deal with a weak immune system. You all want to avoid this path to health problems-- its a lot of work to overcome!
There are many great habits you can form to improve your health: it just takes self discipline— and an informed approach using the best of many different modalities.
So— the entries I have posted under COVID-19 are the best bets I can pass on to INSPIRE you to take up a healthier lifestyle.
You CAN do it-- it is worth the effort...
Corona Virus: Tips from an Immune Pro
The most important things I have learned to keep healthy: Breathing... Yoga... Lifestyle... Outlook.
This section is designed to help you to boost your immune system-- by learning from my experience in dealing with a rare immune condition: "Common Variable Immune Deficiency" or CVID.
When I was finally diagnosed with low antibodies after 32 years of having major symptoms-- my UCSD immunologist Dr Marc Riedl said to me: "You are supposed to have infection after infection after infection!"
I said: I don't-- because I take care of myself. I eat right and I do yoga!
He recently ordered this PFT for me as it is standard test for CVID patients. I told him I had wanted to see if I was still at 130% as I was in 2016. No-- I've improved my Force Vital Capacity (FVC ) by 2%...
My Pulmonary Function Test Result FVC of 132%
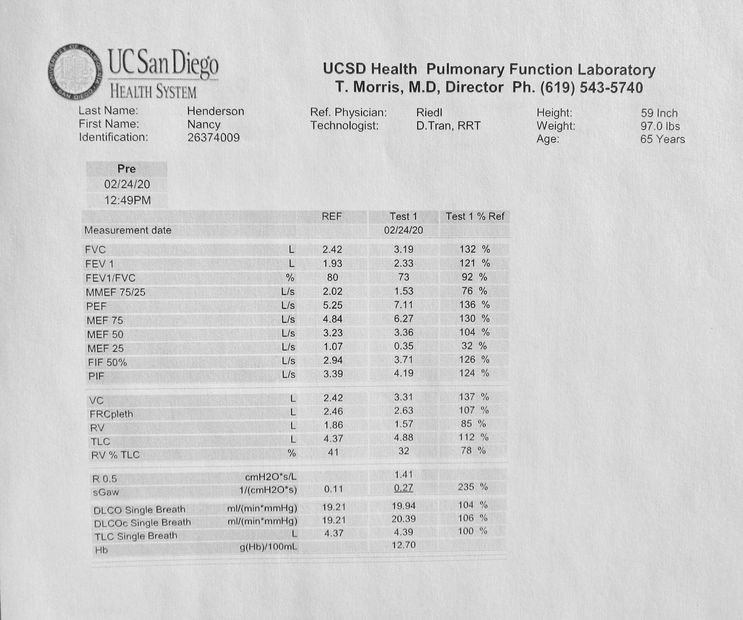
This is at age 65, after 25 years of yoga and 10 years of practice with my breathing prompt.
My pulmonologist called me "Super Woman"-- and said that this is the same result as a 22 year old has. So-- I am doing something right that is counterbalancing the normal presentation of CVID which is chronic respiratory infections. I have also been doing a pranayama based breathing meditation for nearly 30 years.
Parasympathetic Breathing Prompt for Medical Professionals
This is an EXAMPLE of my specific prompt which is unique to me for my very restricted 1 mm airway. For other patients or the general public: Every one is unique-- and a professional with the proper medical equipment would have to create a breathing prompt specifically for them. The way to use it would have to be specific to the recipient as well. This project requires skill and knowledge beyond the average breath-work enthusiast.
(Note-- If this does not download in Safari, try Chrome)
03-25-10 (m4a)
DownloadAt 65-- I am a "Kick Ass Zebra"!

Those of us with CVID are known as Zebras...
CVID-- or Common Variable Immune Deficiency-- is a very rare (1 in 30,000) genetic condition which is characterized by very low antibodies. Before starting treatment about 3 years ago, my IGG's were at 406 compared to the normal range of 700-- 1500. We are unable to fight off infection, and must have immunoglobulins replaced with periodic intravenous plasma. I get replacement every 3 weeks now-- which costs Medicare and my other insurance $5,000.00 to $7,000.00 per infusion! The billed amount is $19,000.00!
Here I am March 29th 2020 doing yoga while getting an infusion at the same time.
The paradox of having a weak immune system is that you need to be VERY strong! I also have other medical conditions-- sleep apnea, SICCA syndrome, Lyme, painful degenerated spinal disks, limited use of my right arm and more. Most of my CVID issues are in the gut. It is in the GUT where most of the immune system lies. I know more than I EVER wanted to know about the immune system and how to support it.
YOU can benefit from the lessons I have learned on how to keep healthy despite the odds.

Here I am at the UCSD Infusion Center December 2019 with my artwork, and a thank you note to my MD's and insurance for covering payouts of $160,000.00 to $256,000.00 in 2.8 years. While usually it is 6-10 years before most people are finally diagnosed with CVID-- it was 32 years for me after major symptoms. This was a kind of Hormetic stress that actually ended up making me stronger. Because of constant pain and stiffness, I am now unable to do most of the work I did in the past: tight detailed illustration or portraiture. But, this beautiful wall sculpture-- which is unique to me-- is still on my "can do" list.
I hope to raise funds for Charity through the sales of my art-- and to have a legal agreement where both the Charity and the Buyer benefit. This will be the way we will need to work post CoronaVirus: close the loop of art from China. So-- think in terms of supporting your local artist! I look forward also to working with artist's reps like ArtLifting. They exclusively represent disabled artists to major corporate clients such as Google.
Here is a 2001 selfie of me in Yosemite at the base of El Cap-- right below a really fun 5.10a climb I led a couple of times way back in the 70's: "Sacherer Cracker". Behind me is a great view of another classic climb on Middle Cathedral that a dear friend -- Maria Cranor-- and I swung leads on: "Pillar of Frenzy." It's 5 pitches of sustained 5.9-- and my memories of an unforgettable view of a helicopter rescue on El Cap-- and one of the scariest descents we ever made: the rope got stuck and it was getting dark, and Maria had no choice but to Batman up to get it-- still remain vivid in my mind. Yeeow!
SO many happy memories in Yosemite as a climber for 17 years.
I even tagged along on a couple of Big Walls with my Ex. He led (and I jumared) on the West Face of Sentinel. Now-- with the effects of the low immune condition--every day feels like a Big Wall-- the amount work I need to do to get thru the day.
I have developed a lot of coping strategies that keep me positive, as healthy as I can be, and ready to help others. I hope you can benefit from my lessons learned. That which does not kill you makes you stronger!
Learn Yoga and Meditation to Help Calm Stress...

This is Potato Chip Rock at Mt Woodson in North County San Diego. For the past several years I have hiked from Lake Poway to the top on my birthday-- as a way to mark the years.
I have to say it IS scary up there-- and non climbers have NO business being up there! But with my 17 years of climbing and my yoga practice-- I go up there to get my "Vertigo Victory" shots. A couple of MVA's left me with a painful neck injury and vertigo-- but my breathing prompt-- plus yoga, weight training, pilates, and postural practice keep it under control. I hope to inspire others to maintain a daily health and fitness routine.

Can you see the mass of people waiting to get their hero shots? You have to wait in line now for an hour to be able to get your hero pose on top!

I'm no different! Here I am just before my 65th birthday! I have to work so hard to overcome pain and stiffness from the CVID-- that the side benefit is a level of fitness you don't see in most "seniors."
More Benefits of my Parasympathetic Breathing Training...
I created my Parasympathetic Breathing Prompt 10 years ago (with the assistance of a medical device and specific training) in order to keep myself awake in my truck. I was falling asleep due to severe sleep apnea, and my complex 90K surgery was a couple of years away-- the soonest my SS Disability would come through.
It not only helps my brain to keep alert and my body less fatigued by feeding in the correct amount of O2-CO2 mix...
But-- it is a very useful adjunct to meditation as it paces the breath.
It helps anxiety reduction as it teaches parasympathetic breathing.
It helps to keep me paced-- so that I do not move any faster than I can comfortably breathe with it.
I used to have asthma all the time and rarely do now.
I think it has helped with my OSA-- as my AHI is usually under 1.
It helps mask tinnitus and I wear it all the time because of this alone.
It helps with vertigo as it is a "4th anchor."
It helped me to go thru 3 procedures and 4 surgeries w/o sedation:
2 pterygium surgeries
2 hand surgeries
A colonoscopy, a sigmoidoscopy and an endoscopy.
(The Anesthesiologists who were in surgery were very complementary)
Dr Heikel my UCSD Shiley Eye Center surgeon wants me to teach his pts-- so they can remain alert during surgery and be able to cooperate with his direction to move their eyes in various poisitions.
It has application for post surgery when a cumbersome breathing tool is brought by to exercise the lungs. Nurses that observed me using it post appendectomy were impressed.
I have been wanting to market it-- but hurdles have been in my way-- and people discount breathing.
But now with the interest in avoiding COVID-19 -- I think it is time to get it out there.
I welcome Medical Professionals to contact me for further discussion and to brainstorm ways we can begin to use this concept to individualize breathing training for patients and the general public.

What is Parasympathetic Breathing? It Helps with Stress:
1-- It begins with breathing through your nose--
NOT your mouth.
Your nose is designed to warm and humidify the air, and to filter particles out before they get into the lungs.
2-- Breathe in through your "belly."
According to Lung.org: " Humans are Belly Breathers," and just above your stomach is a major muscle in the respiration process, the diaphragm. Proper breathing starts in the nose and then moves to the stomach as diaphragm contracts, the belly EXPANDS and fills with air. "It is the most efficient way to breathe as it pulls down on the lungs, creating negative pressure in the chest, resulting in air flowing into your lungs."
3-- Understand your Autonomic Nervous System has two critically intertwined sides that work together as a single unit.
In short:
On the INHALE your Nervous System is in Sympathetic mode.
On the EXHALE your Nervous System is in Parasympathetic mode.
Sympathetic is Energizing: "Fight or Flight".
Parasympathetic is "Rest and Digest"
Like the symbol of Yin and Yang they seem to be opposites-- but actually each side contains a small portion of the other. They are complementary rather than opposing forces. And more importantly, they are imbedded in the Circle that represents the Greater Whole.
Respiratory Therapist Rosemary MacGregor, RN, told me when she coached me years ago that
O2 and CO2 are PARTNERS in oxygenation. This is counter-intuitive to most Yoga practitioners-- because we have all been told:
"In goes the good air-- out goes the bad."
But, it's not so simple.
She said most of her clients did NOT get this rhythm balanced correctly-- and they were constantly in a chronic stress response: Sympathetic overload.
Most people are subtly hyperventilating most of the time. They are INHALING too much oxygen and not EXHALING enough CO2.
Therefore-- the normal balance of opposites-- even breathing-- where the inhale is the same length as the exhale needs to be corrected.
Lois Laynee of RestoringBreathing.com in Dr Steven Park's 2012 podcast explains that:
"Inhalation gets air to lung and oxygen to blood...."
"Exhalation gets oxygen to the brain and muscles"
"Exhalation removes waste gases"
She goes on further to explain:
"ABSORPTION OF OXYGEN:"
"Inhalation allows the air thru the airway, to the lungs for absorption of oxygen into the blood.
INHALATION FOR A COUNT OF 3."
"Exhalation allows the delivery of oxygen to the tissues and most importantly to the brain."
"EXHALATION FOR THE COUNT OF 5-- OR IDEALLY 6"
___________________________
So-- the breath-work practitioners that teach you to take in a large breath-- and HOLD it before a shorter exhale are stressing your sympathetic nervous system and keeping you in flight or fight.
The oxygen does not get completely delivered until you fully exhale.
To get you into Rest and Digest-- Parasympathetic mode-- you will need to exhale fully and IF you hold-- it should be at the bottom of the exhale.
Lois Laynee on Dr Park's podcast teaches a 1-2 breathing style-- the inhale is half as long as the exhale. You can stretch this out for different applications which I discuss later. Many breathing techniques exist. Some seem to contradict one another. This is a rich subject, but these are the basics here for Parasympathetic Breathing which you need to know for times of stress:
1-- Nose Breathe
2-- Expand Breathing into the Belly
3-- Longer Exhalation
A 4th addition: Breathing through your nose with a long exhale also creates Nitric Oxide-- which delivers more oxygen to your tissues.
Here is a link to the interview with Lois Laynee on DrStevenPark.com's Breathe Better Sleep Better site:
https://doctorstevenpark.com/?s=lois+laynee&submit=Search
Constantly being in Sympathetic Overload because of poor breathing habits is one of the MOST detrimental habits that can undermine your health. This can be happening both day and night. The best way to get out of Sympathetic Overload is to train yourself to breathe properly...
Please use this Parasympathetic BreathWalking Infographic I
See COVID #2 for a detailed explanation of these principals
Download PDFMore on Breathing Techniques...
Wim Hoff Breathing: not for the average person. Dr John Doulliard of LifeSpa says his technique is "like taking Prednisone."
His ideas are based on Hormesis-- stressing the body to make it stronger. His use of Cold Thermogenesis along with a stressful breathing technique is the combination that works. Cold Thermogenesis is impressive-- and Wim is known as "The Ice Man" for good reason.
I am more impressed with the medical expertise of Patrick McKeown in being able to explain breathing. Patrick's work is used for asthmatics. Both use different breathing techniques that challenge/stress the lungs in a more dramatic way to make them stronger, and feature breath holding.
Both are for extreme situations.
The way I was taught by Rosemary McGregor was less dramatic-- producing less immediate results than say Patrick's method. She did not advocate breath holding as she said it was a bad habit you should strive to overcome. So-- the breathing prompt idea is to slowly build up your ability to breathe as efficiently as possible using entrainment of the breath. Think of this as an every day all day approach. This technique is what has allowed me at age 65 to have the pulmonary function of a 22 year old.
Assistance from a trained specialist with special medical equipment is necessary to find your best breathing rate and ratio.
However-- this technique-- and much of the benefit can also be done with attention to the breath while walking or jumping on the rebounder.
The Infographic above is a great way to practice this "less dramatic, every day" Parasympathetic Breathing technique. The idea is to create a conscious breathing pattern that you can keep up for long periods of time-- one that expands your ribcage and facilitates better breathing both day and night.
Breathing Easier about Corona Virus....
The COVID-19 virus attacks the lungs.
Therefore-- BREATHING is #1:
In my opinion-- the most IMPORTANT thing you can do is to work on your ability to breathe freely both day and night. After all-- how long can you last without oxygen?
And, understanding the basics of how breathe while under stress will help you avoid anxiety, too.
You MUST make sure you are nasal breathing both day and night
if you want to have a strong immune system
and good pulmonary function.
In an Emergency- Think A B C: Airway, Breathing, Circulation
Recommended Websites:
DrStevenPark.com-- his theme: "Breathe Better, Sleep Better"
"10 Ways to Combat CoronaVirus" many great podcasts
Get his free e-book on How to un-stuff your stuffy nose.
On his site-- search "Lois Laynee" for a great A/V presentation
Lois Laynee-- RestoringBreathing.com
Several great (but technical) podcasts
Parasympathetic breathing,
Why you need to learn to hum (great podcasts)
Patrick McKeown-- Buteyko Breathing
" Is Breathing Your most important defense against Corona Virus?
https://buteykoclinic.com/corona-virus/
Search his Free Children's Breathing Link
NoseBreathe.com: Dental Appliances (day and night)
Very important concept to understand why you need to train
the tongue forward and open the airway.
__________________________________
How to support better breathing with CoronaVirus:
DO A DEEP SPRNG CLEANING FOR YOUR HOME:
Check your Home for airborne pathogens--- mold especially.
You may not be able to breathe freely because of poor indoor air quality. 25% of people have severe mold sensitivities and some don't realize it. It may be linked to behavioral problems as well. During smog season and our California fires here I am unable to go outside.
I need to live in a "clean room" environment. It has been my experience that when I am around airborne allergens, molds, chemical toxins-- that my breathing is short and l cannot think clearly. Many people have this as well-- but they experience anxiety and do not know why. They go into a Sympathetic overload just from their body's natural aversion to airborne pathogens.
I call this the "Smell Danger Response".
It takes more than learning how to manage stress-- you need to remove the source of the stressful pathogens, so you can think clearly enough to function.
Learn more here-- look for COVID-19 posts:
ISEAI.org International Society for Environmentally Acquired Illness
SurvivingMold.com
Fans and a dehumidifier will go a LONG way to reduce pathogens in your home. Keep your humidity at 50%. Remember that pathogens do not like sunlight and air circulation.
Studies show that Air Quality inside the home is worse than outside.
"Either buy a filter-- or BE a filter."
HEPA Hospital Quality Air Filtration system I use:
IQ Air https://www.iqair.com/us/
(this may be considered DME by your insurance)
THIS UV LIGHT MACHINE KILLS MOLD AND VIRUSES-- even COVID and MRSA:
"Air Reactor" https://www.hitechairsolutions.com
(please let them know I referred you if you purchase)
OZONE KILLS PATHOGENS-- I drink ozonated water every day-- and use this in my nasal rinse after going out in a congested public space.
An excellent product which has improved my health:
Longevity Resources https://www.ozonegenerator.com
Inspiring information on Ozone Therapy:
DrRowenDrSu Clinic is accepting COVID patients
Dr Rowen and the Ebola Virus in Sierra Leone-- search Dr Mercola.com podcasts.
(Note I do not advocate the use of other home Ozone generators ("Alpine Air") to clean your air while you are IN the home as ozone can irritate the lungs. Use them while you are OUT of the home and then air out afterwards.)
Make your Bedroom a Sleep Sanctuary:
Go through all of your bedding and keep it clean.
Dust mites can account for 10% of the weight of your pillow after 2 years!
Protect your bedding with dust mite proof coverings.
Allergy proof all of your home. Ideally-- get rid of carpeting and all other dust collecting surfaces which can be a home for pathogens to live in.
Practicing Balance using my Breathing Prompt
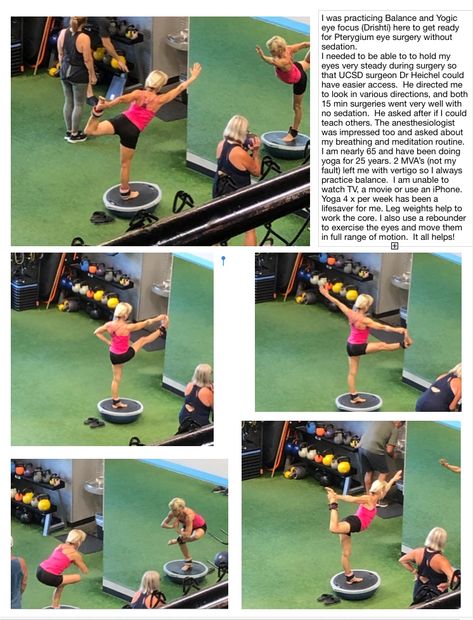
And practicing my Yoga Gaze "Drishti" for eye surgery and my Vertigo Victory shots...
I have been able to go through 4 minor surgeries , a colonosopy, sigmoidoscopy and endoscopy without sedation because of the focus I have learned from my yoga and Breathing Prompt practice. This Breathing Prompt is a 4th Anchor for balance-- along with the eyes, inner ear and proprioceptors. My UCSD Shiley Eye Center eye surgeon asked me if I could teach others to be awake during surgery. Yes. It would be very helpful for many procedures if the patient could be trained to get over some anxiety. These photos were taken in August 2019 by a dear RN friend who I have known for over 20 years at "Frogs" gym in Encinitas. Thank you Rebecca!
BREATHE LIKE A SHERPA AT HIGH ALTITUDES
by Rosemary MacGregor, RN, MS Photo Credit: API
Summary: It is basically breathing in through the nose, not holding, and a longer exhale with pursed lips. This is the way the Sherpas breathe at high altitudes for long periods of time…
The right breathing took a group of trekkers to the top of the world.
In April of 1989, 10 mountaineers left for a trek to Everest base camp in the Himalayas to test my theory on breathing. This first trek was a preliminary study to see if my beliefs about breathing were correct.
I started by placing ads in the The Mountaineer magazine in October 1988 with the hopes of recruiting 10 brave adventurers for the trek. They would be trying a method of breathing that was different than that being advocated and done by many experts, some who made it to very high altitudes and others who did not.
One individual joined the group late and only had three weeks to prepare. He did not get the same training and in essence could have been considered a control. This participant was a marathon runner and aged 24. All others received at least three months of breathing training.
Each of the nine trained individuals came to my office for group instruction, was hooked up to a biofeedback breathing tracer, was taught how to breathe properly and was subsequently tested while exercising with a capnograph, a machine that measures arterial blood C02 levels.
Four of the individuals were taken to Harborview Hospital’s pulmonary lab, where they were each put through a respiratory challenge test. Each was subjected to a hypoxic challenge, comparable to ascending to 14,000 feet in five minutes (top of Mt. Rainier), to a CO2 stimulus (a potent challenger to breathe) and finally to a maximum exercise condition.
Dr. Browne Schoene, head of this lab at Harborview Hospital in Seattle, Washington and head of respiratory medicine at the University of Washington was of the belief that you could not control breathing under such adverse conditions. I was of the belief, that with proper training you could indeed improve respiration under such challenges. In each of his challenges, O2, CO2 and max exercise, each one of the four trained “trekkers” was able to demonstrate that with controlled and a much slower respiratory rate that they were able to yield oxygen levels comparable to top-quality athletes.
We left for Nepal on April 6, 1989. It was my intention that this breathing technique would get us to Everest base camp or above with less difficulty than most trekkers or climbers who had never learned a new way of breathing. I had never done any trekking or mountain climbing myself and knew that less than half those intending to make it to Everest base camp made it. I left questionnaires at the Sagarmatha Park entrance for other trekkers to fill out to access their symptomatology and considered they would be like a control group.
I was able to obtain two instruments to be used as biofeedback machines. One was a capnograph. This machine measures the amount of CO2 in the alveoli and this is essentially the same as that found in arterial blood. The second machine was an oximeter, which tells how saturated is the arterial blood with oxygen. The capnograph would give us more telling information than the oximeter. Unfortunately, we had to leave the capnograph behind at 11,200 feet due to cold temperatures. It would not work in very cold temperatures.
Our group used a small, tape recorder sized Criticare Systems oximeter. Each person was to carry this around their neck for ½ hour twice a day. They were to obtain and record O2 saturation readings and make adjustments as needed during that time period. They also filled out a diary twice a day. The questions were very similar to those asked of the “control Sagarmatha Park trekkers”.
Subjective assessment (O2 readings) did prove to be latent and breathing needed to be modified as ascent was made. The oximeter was a very helpful tool in recognizing the need to increase breathing but it did not tell us breath by breath if we had enough C02 on board to unload O2 to the tissues. Had we been able to carry the capnograph with us we could have had more accurate information. The oximeter simply gave us feedback as to our O2 saturation levels. Since acclimatization takes up to 48 hours to take place, the body does not make the important and needed adjustment and, at the same time we were always climbing higher, except at rest and nighttime. The body does not accurately sense the need to breathe more. We were always 1 step ahead and two behind in our oxygen needs. Essentially, we were doing biofeedback using an oximeter to monitor our O2 levels while ascending the terrain. We did take a capnograph with us to monitor C02 levels but found it would not work properly in the colder temperatures of the mountains. Ideally, one should have both. If I had to choose one I would most definitely pick a capnograph. It is the more telling instrument for this endeavor.
Katmandu, Nepal sits at close to 4500 feet elevation. We flew from Katmandu to Lukla at 9,300 feet and slept overnight at Phadking at 8,700 feet. We were not acclimatized when we set off the next morning for Namche Bazaar at 11,200 feet. At Namche we stayed for two nights to catch up on our acclimatization. Many don’t realize that altitude sickness can happen at 9,000 feet and this prevents many skiers and climbers from ascending any further or skiing in the mountains of Colorado.
The last hours of our second day proved to be most difficult. We had ascended 2500 feet to a horseshoe shaped village Lukla, on the side of the mountain. Normally the recommended ascent per day is no more than 1000 feet. The body can adjust to this, but, in Nepal the ascent from Phakding to Namche Bazaar is standard and very difficult. Then, a two day rest at Namche is recommended and allows for adjustment and acclimatization to take place. If one is prone to altitude sickness it usually shows up at this point. In our group, one person failed to keep hydrated and nearly passed out, and another commented that this was the most humbling day of her life. In truth, this stretch from 8,700 feet to 11,200 is reportedly one of the most difficult. It is long, steep and very tiring on top of not being acclimated. Altitude sickness can easily show up if it is going to.
The signs of altitude sickness are fairly visible. You don’t look good, facial and finger swelling occurs, and a screaming next morning headache (like a hangover) are all very common. Vomiting, lethargy, coughing, cerebral and pulmonary edema are less frequent, but are increasingly dangerous signs of a need to immediately descend. As soon as descent is achieved the symptoms disappear.
The untrained 24 year old marathoner developed acute symptoms, and proceeded to bless us with vomiting over the breakfast table. While he kept saying he was ok, obviously this was not true. My daughter, who was on the trek had an acute reaction to phenol from her new REI sleeping bag, outdoor clothing, new plastic water bottle, cough drops and a couple of other items. In her weakened condition she came down with the Kumbu virus, a very debilitating respiratory virus that eventually caught up with the rest of us. The immune system does not perform normally at altitude and infections can occur more rapidly and be slower to heal. As a group these two members were voted to return to Katmandu. A friend of my daughter’s decided to accompany them.
The rest of us set off for the monastery of Tangboche at 12,000 feet. We were teary eyed and I was especially worried about my daughter. She ended up in the hospital in Katmandu for 6 days. Breathing was getting more and more challenging for the rest of us. It became evident that there could be no slacking or non-engagement of the breathing technique. At this altitude, every step is precious and requires max oxygen. The oximeter was incredibility helpful in giving us feedback as to our performance. Without this feedback, we tended to under breathe. In looking back, I feel there was a very fine line between under and over breathing. With this twice a day feedback, on the average we were able to catch our bodies up to the on-going ascent and keep our oxygen saturation levels at 85% or above.
Before making this trip I did research, went to the International hypoxia meetings, talked to many experts and doctors and found no one talked about breathing training. Some recognized the Sherpas of Nepal breathed differently but it was never appreciated or looked at as something to learn from. I have since noted that Doctors do not look at behavior, only blood gases. I felt that ego ruled the day in most cases. There were a few exceptions that I knew of, like Reinhold Messner and Tim McCarthy Snape who both scaled Everest twice without oxygen.
“Born in Tanzania (Africa) in 1956 to an Australian mother and a British father Macartney-Snape has made numerous ascents of the world's tallest mountains in classic lightweight style without bottled oxygen. In May of 1990 Macartney-Snape became the first person to climb the full height of Everest from base camp to summit without oxygen, Sherpa support or fellow climbers. This three-month climb was immortalized in the award winning film "Everest: Sea to Summit".
Dr. Thomas Hornbein (first American to climb Everest) and the American Everest Expediton of 1984 were all aided by a great entourage of Sherpas and oxygen bottles. Yet, few of the Sherpas used oxygen. Rather than looking at their breathing behavior, these experts concluded that the DNA of the Sherpas was different.
Having worked with these two Drs, Schoene at Harborview and interviewing Dr. Hornbein at the University of Washington, it was my conclusion, that like many other areas of their repertoire, their egos got in their way and told them that whatever they did (how they breathed) was right and subsequently based all their conclusions on this. More on this later.
On this Everest Base camp trek we passed many trekkers. I noticed them standing up straight, carrying heavy back packs and very visibly hyperventilating. Why? Being an expert in stress, I could see that they were in a severe stress response. Conditions were very stressful and they were responding accordingly. They had not undergone any training to override this. This was a max stressful environment and very demanding on the human body. What does the body do naturally in this situation? It will hyperventilate. On the other hand, the Sherpas did not hyperventilate. They had lived in these conditions, adapted to them and learned how to respond differently. They did not stand up straight or carry a backpack of 35-75 lbs. No, they bent forward, carried up to 150 pounds in their basket on their back and instead of open mouth hyperventilating, they pursed lip breathe, made a funny little whistle sound and sometimes even sang and danced on the way up the mountains. In bending over and carrying weight on their backs (not shoulders), they naturally diaphragmatically breathed and could carry more weight. They carried their baskets via a tompa band that goes around the baskets and forehead.
Western climbers were hyperventilating, high chest breathing and blowing out too much CO2 too quickly. Dr. Schoene and Dr. Hornbein confirmed this with me in an interview prior to our trip. I felt the tiny minute difference between pursed lip exhalation and open mouth exhalation made the difference between successful ascent and mountain sickness. I met Tim McCartney Snape on his way down Mt. Everest and he confirmed that this was the technique he used. I met him in Lukla and then again interviewed several years later in Australia.
I tried to point out to Drs. Schoene and Hornbein that chest breathing was not the breathing of choice for ascent. If they would look at the Sherpas they would notice that they did not chest breathe. They bent over and in that position it is nearly impossible to chest breathe. I tried to point out that chest breathing induced a stress response and that was the last thing one needed on top of the imminent already stressors of high altitude.
Before leaving for Nepal I attended the International hypoxia meeting in Baniff, Alberta in 1988. I met some wonderful mountaineers and doctors who were interested and supported my theory. I was a pioneer introducing the idea of learning to breathe properly to climb to altitude. Why should this be so strange. Divers have to be in touch with their breathing, as do weight lifters, swimmers and runners. The very best athletes are the very best breathers. In doing research on breathing at altitude, there was nothing published suggesting or insisting on a need to breathe differently or like the Sherpas. Eastern cultures have talked about breathing for thousands of years. Herbert Bensen at Harvard mentions the breathing the high lamas do to perform Tomo yoga, the basic requirement of breathing to do meditation, as well as the many Olympic athletes (especially Russian and Chinese) to excel at performance. I had been using breathing training in biofeedback for over ten years with my clients and saw more positive results from breathing than any other technique. Pioneers pay a price when introducing new information that goes against conventional public opinion and ongoing research.
My initial library searches on climbers and breathing techniques only yielded information on hyperventilation as the consequence of climbing to altitude. Dr. Schoene actually recommended it and was doing research and writing papers on this. I observed a video of Dr. Thomas Hornbein hyperventilating (could see his chest heaving) on his initial climb to the top of Everest. He invented the oxygen machine for climbers. On the 1984 American Everest Expedition, Dr. Peter Hackett was said to be breathing 85 times per minute on his last leg up Mt. Everest. There are only 60 seconds in a minute.
I was shocked when I read this information. The hyperventilation I was seeing was stress breathing, a very normal response to acute stress but not necessarily the desirable one.
To me hyperventilation consists of two things: high chest breathing and excessively fast breathing that blows off too much carbon dioxide too quickly. This was the definition Dr. Hornbein had shared with me. Obviously, faster breathing was required at altitude, but did the exhalation need to be that fast (with open mouth) and did it need to be in the chest? What if, like the Sherpas, the climber took in a deeper breath using the diaphragm and blew it out through pursed lips more slowly making the whistle sound like the Sherpas. This would raise arterial CO2 or prevent such an immediate loss. The slightly higher level of C02 would prevent the vasoconstriction of the cerebral, coronary and peripheral arterial system. I had wondered about cerebral and pulmonary edema and cold hands among climbers. Dr. Brian Tiep had done research on using pursed-lip breathing at altitude and shared with me that this would drive more oxygen into the system. This is what the Sherpas were doing.
Now, back to the trek. After two days acclimatizing at Namche Bazaar, we set off for Tangboche at 12,000 feet. Breathing was getting more difficult. We needed to pay more attention to our breathing, monitor ourselves and fully attend to each breath. Without the feedback from the oximeter, we tended to under breathe. With the feedback we were able to keep our oxygen saturation levels on an average of 85% while trekking and above 90% while resting. By using the oximeter to guide our breathing, we seemed to keep one step ahead. Not everyone used the instrument every day twice a day. In looking at the data upon our return I noted that those who did not used the instrument religiously twice a day were the ones who had more symptoms. One of our members woke up at Pangboche (13,000 feet) with a screaming headache. This is quite common among climbers. He also had facial swelling. He desperately wanted to continue, so I sent him to go sit down, do his breathing consistently and use the oximeter for feedback. He did this for 30 minutes, said his headache was gone and he continued with us, religiously doing the breathing every step. He made it to the top of Kala Patar, around 20,000 feet. With normal climbers these headaches are almost a daily occurrence and don’t go away quickly like ours did. We found that by gaining the feedback from the oximeter, adjustments could be made and the headache would be gone in about 10 minutes.
We all made it to Kala Patar before the noon winds of 40-50 mph. The view of Mt. Everest was spectacular with its halo of clouds behind its majestic midnight blue peaks. We were above Everest base camp looking down on it and the Kumbu glacier or icefall.
It was time to descend. The oximeter and breathing training had taken us to great heights registering O2 saturation levels of 80-95%. This was much higher than the average climber or trekker. Also, our overall symptomatology was significantly less than those who filled out and returned the questionnaires to the Sagarmatha Park attendee.
Some interesting symptoms occurred on the descent. The pace going down is quite rapid in comparison. There was a lot of stumbling and lightheadedness. Many complained of headaches. When I checked my own oximeter oxygen level I was down in the 60-70% range. None of us were paying the same attention to our breathing as we had while ascending. We were still breathing the same air though and our bodies had not adjusted to the level of oxygen with our increased level of exertion.
Now, a few words on the breathing method. Altitude and sea-level breathing are different. Without training, I believe a person will automatically experience altitude as a stressor and resort to chronic hyperventilation. We required months of training. We practiced the breathing technique hiking in the lower hills of Washington State and one trip up Mt. Rainier. We had to be very conscious of our breathing. Besides the deeper breathing using the diaphragm, the whistle breathing of the Sherpas did in fact immediately increase our oxygen saturation. We were not blowing out as quickly as well and kept more CO2 on board allowing our hemoglobin to offload more oxygen. More force is required to whistle breathe and this leads to a greater back pressure, allowing for more oxygen exchange.
Dr. Schoene was most interested in my results which I generously shared with him. After submitting my material to Dr. Houston, editor of the Alpine journal, both Dr. Houston and Brownie Schoene cut me off and would not even talk to me. It was several months later that Dr. Bruce Patton sent me a copy of the NEJM article, the rewriting of the 1984 American Everest Expedition with new explanations based on hypocapnia, or low C02 They had used my information and material to rewrite their 1984 expedition and also to publish this in the NEJM in an article on “Hypocapnia”. This only confirmed for me that knowing the C02 level was more important than the O2 level.
I made a second trip with 14 individuals the next year and this trip resulted in a 7 year court battle over this information that went all the way to the Washington Supreme Court. That is a whole other story.
Rosemary MacGregor RN, MS
A Note about Rosemary’s Article...
She passed before her work was done. Too bad her site was not kept going. She had a book she wanted to publish— (Change Your Breathing— Change Your Life) I was trying to help her with it and then also market my breathing prompt. People just don't want to work at breathing when it is something they already do. They just want a pill and no work involved!
The above was a chapter from it...
